Enhancing Opioid Use Disorder Treatment with App-Based Contingency Management
A recent JAMA Network Open study found that patients who used WEconnect alongside their MOUD treatment had 35% fewer days of opioid use and stayed in treatment nearly two months longer than those using MOUD alone.
Executive Summary
The opioid addiction crisis remains a pressing public health emergency, demanding innovative approaches to improve treatment outcomes. Medication for Opioid Use Disorder (MOUD) – such as methadone, buprenorphine, or naltrexone – is the evidence-based standard of care for opioid use disorder. However, many patients continue to struggle with relapse and retention in treatment, indicating a need for complementary interventions. A May 2024 study in JAMA Network Open provides compelling evidence that augmenting MOUD with a digital contingency management (CM) program can significantly enhance patient outcomes. This white paper summarizes the study’s key findings and explores their clinical and economic implications, positioning WEconnect Health as a leader in delivering scalable, app-based CM in addiction treatment. It is intended for healthcare providers, payers, and policy stakeholders seeking effective, technology-enabled solutions to combat the opioid epidemic.
Key Highlights:
- Evidence-Based Improvement: New research shows that patients receiving MOUD plus app-based contingency management had about one-third fewer opioid use days by end of treatment and stayed in treatment significantly longer than those on MOUD alone. In the study of 600 patients, the app-supported group reported 8.4 days of opioid use vs 12.0 days in the MOUD-only group, and remained in treatment for 290 days vs 236 days on average – a 35% reduction in use days and nearly 20% longer retention than standard care.
- Clinical & Economic Impact: Reducing opioid use and improving retention translates to better health outcomes and potential cost savings. Fewer opioid-use days mean lowered risk of overdose and transmissible infections, while longer treatment engagement is linked to higher likelihood of long-term recovery. Given the staggering annual societal cost of the opioid crisis (almost $969 billion in 2018), even incremental improvements in abstinence and retention can yield substantial public health and economic benefits. MOUD alone already confers cost-saving benefits by reducing morbidity and mortality; adding digital CM can further amplify these benefits.
- WEconnect Health’s Digital Solution: WEconnect’s smartphone app delivered the CM program in the study, demonstrating how technology can overcome traditional barriers. The app provides financial incentives for meeting personalized recovery goals and integrates peer support and progress tracking into a single platform. By leveraging a digital contingency management approach, WEconnect Health offers a scalable, high-fidelity intervention that can engage patients anywhere, anytime – increasing access to evidence-based support beyond the clinic setting. This positions WEconnect as a frontrunner in digital addiction treatment, uniquely equipped to help healthcare systems and communities implement contingency management at scale.
- Call to Action: The findings call for broader adoption of digital CM in opioid treatment programs. Healthcare providers and treatment centers should consider integrating app-based CM alongside MOUD to improve patient outcomes. Payers and policy-makers are encouraged to support and reimburse digital therapeutic platforms like WEconnect, given their demonstrated ability to enhance retention and recovery success. WEconnect Health stands ready as a partner in deploying these digital solutions, which can be rapidly scaled to expand access, reduce costs, and ultimately save lives in the opioid epidemic.
Introduction: The Opioid Epidemic and the Role of MOUD
The United States continues to face a grave opioid use disorder (OUD) epidemic, with tens of thousands of overdose deaths each year and profound social and economic consequences. In 2018 alone, the opioid crisis carried an estimated $968.9 billion in societal costs in the U.S.. Beyond financial impact, opioid addiction has devastated families and communities across the country. Effective treatment strategies are urgently needed to curb this crisis.
Medication for Opioid Use Disorder (MOUD) – including methadone, buprenorphine (Suboxone®), and extended-release naltrexone (Vivitrol®) – is widely recognized as the gold standard treatment for OUD. Indeed, MOUD is “the only evidence-based treatment” for opioid addiction, significantly reducing opioid-related morbidity and mortality and yielding consistent cost-saving benefits. Patients on MOUD have markedly improved outcomes compared to those not receiving medication. However, MOUD alone is not a panacea. Many individuals on MOUD continue to face challenges such as breakthrough opioid use, cravings, and difficulty adhering to treatment plans over the long term.
One critical issue is treatment retention – keeping patients engaged in care long enough to achieve lasting recovery. On average, fewer than 20% of individuals with substance use disorders receive any treatment at all, and among those who do, dropout rates can be high. Patients often struggle with psychosocial stresses and triggers that medication alone may not address. As a result, some MOUD patients experience difficulty reducing opioid use and staying in treatment, highlighting the need to augment MOUD with additional support. In many areas of medicine (e.g. depression, diabetes), combining medication with behavioral therapy yields better outcomes; similarly, opioid addiction treatment may benefit from adjunct behavioral interventions.
Contingency Management (CM) has emerged as an effective behavioral strategy to reinforce sobriety and treatment adherence. CM is a therapy approach that provides positive incentives (rewards) for accomplishing specific treatment-related goals or behaviors. In the context of OUD, this often means offering modest financial or prize incentives for objective evidence of abstinence (e.g. negative opioid urine tests) or for meeting recovery milestones. A robust body of research identifies CM as “one of the most effective, evidence-based treatments for substance use disorders”. Several clinical trials and meta-analyses have found that patients receiving CM alongside MOUD have better retention in treatment and higher rates of drug abstinence than those receiving medication only. In short, rewarding positive behavior works – patients are more likely to stay engaged and meet their recovery goals when those achievements are immediately reinforced.
Despite its proven efficacy, traditional contingency management has practical limitations. Historically, CM programs require patients to attend frequent clinic visits (often multiple times per week) to submit drug tests or report progress, so that rewards can be dispensed. This intensive in-person schedule creates barriers for many OUD patients, who may lack transportation, live far from clinics, or juggle work and family responsibilities. The COVID-19 pandemic further highlighted these challenges: many patients became unwilling or unable to attend in-person appointments for CM during lockdowns. These barriers have meant that, until recently, CM was not widely implemented outside of controlled trial settings, even though it is highly effective. There has been a growing recognition that new delivery models – such as telehealth and mobile technology – could make contingency management far more accessible by overcoming geographic and logistical obstacles.
Fortunately, digital health innovations are now enabling contingency management to reach patients in their everyday lives. With the ubiquity of smartphones, there is “an unprecedented opportunity to use this technology to deliver [CM]” to more people in need. By automating the process of tracking recovery activities and delivering rewards through a mobile app, technology-enabled CM can maintain fidelity to the evidence-based protocol while drastically reducing the burden on both patients and providers. This sets the stage for integrating digital CM into standard opioid treatment programs, combining the power of MOUD with the engaging support of a smartphone app. The following sections summarize a new study that evaluated such an approach and discuss its implications for clinical practice and health policy.
Study Summary: App-Based CM Yields Better Outcomes in MOUD Treatment
A recent peer-reviewed study published in JAMA Network Open (Marino et al., 2024) provides real-world evidence for the benefits of adding a smartphone app-based contingency management program to MOUD. The study was a retrospective cohort analysis conducted in Texas, examining treatment outcomes for uninsured or underinsured adults with OUD who had the option to use a recovery support app in addition to their medication treatment. Key details of the study design and findings are summarized below:
- Study Design: Researchers analyzed patient data from November 1, 2020 through November 30, 2023, drawn from several opioid treatment programs and office-based addiction clinics across Texas. The cohort included 600 individuals (≥18 years old) receiving MOUD for opioid use disorder. Participants fell into two groups: 300 patients received MOUD only (standard care), while 300 chose to receive MOUD plus contingency management delivered via the WEconnect smartphone app. Importantly, this was not a randomized trial – patients self-selected whether to use the app – but both groups were comparable in demographics (mean age ~38, ~57% male). All patients were uninsured or underinsured, a population often underserved in addiction care.
- Intervention (App-Based CM): Those in the MOUD + App group downloaded and used the WEconnect Health mobile application as a complement to their medication treatment. Through this app, patients could earn monetary incentives by achieving recovery goals that they set for themselves. For example, a patient might earn small rewards for submitting negative drug screens, attending counseling or support group meetings, or completing healthy activities (exercise, journaling, etc.) that they committed to in the app. The WEconnect app monitored these activities and automatically dispensed rewards (typically in the form of gift card credit) when goals were met, following established CM principles. This allowed contingency management to be delivered remotely, without requiring frequent clinic visits. Patients in the MOUD-only group did not receive these app-based incentives or related digital support.
- Outcomes Measured: The study focused on two primary outcomes: (1) days of opioid use at end of treatment, as self-reported by patients, and (2) treatment retention, measured as the number of days the patient remained in treatment (from initiation of MOUD to either discharge or last follow-up). The end-of-treatment opioid use days essentially indicates recent drug use (lower is better), while retention reflects engagement in care (higher is better). The researchers hypothesized that adding the app-based CM would be associated with fewer opioid use days and longer retention, compared to MOUD alone.
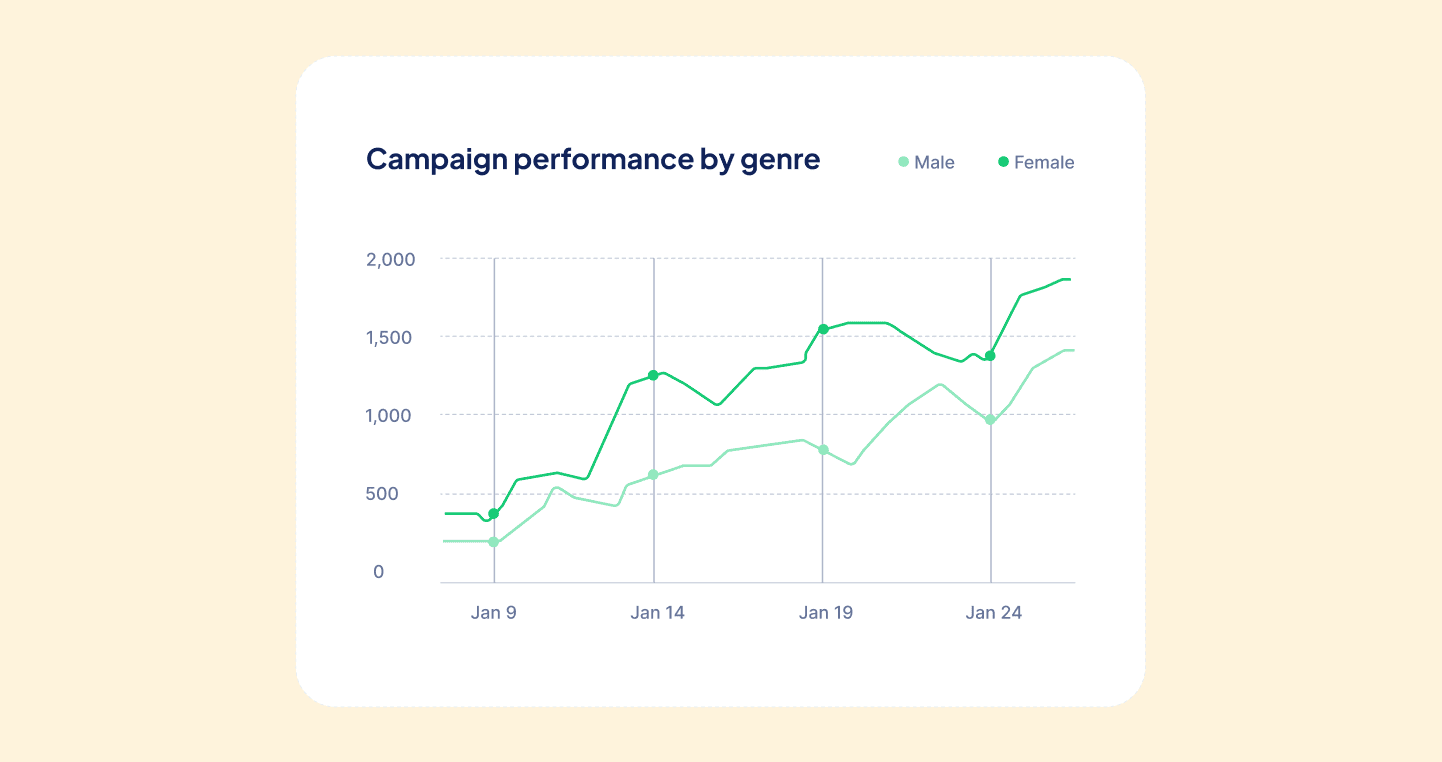
- Key Findings: The results were striking. Patients who chose MOUD + App-based CM achieved significantly better outcomes on both measures than those who received MOUD alone. By the end of the treatment period, the app users reported far fewer days of opioid use than non-app users. Specifically, the MOUD+App group averaged 8.4 days of opioid use, compared to 12.0 days in the MOUD-only group. This represents roughly a 30%–35% reduction in opioid use frequency for those using the digital CM support. In addition, treatment retention was substantially longer in the app-supported group: on average, 290.2 days in treatment versus 236.1 days for the MOUD-only patients. In other words, patients with the app stayed in treatment about 54 days longer (over seven weeks more) than those without the app. The study’s statistical analysis confirmed that these differences were highly significant, not due to chance – in fact, using the app was associated with a β = –6.10 (95% CI –8.09 to –4.10) for reduced opioid-use days and β = +51.91 (95% CI 33.86 to 69.95) for increased days retained in treatment. No serious adverse events or safety concerns were noted, and the intervention was well-tolerated.
Figure: Outcomes from the study by Marino et al. (2024), comparing standard MOUD treatment vs. MOUD augmented with the WEconnect app-based CM program. Patients who used the WEconnect app (green bars) had significantly fewer opioid use days by end of treatment and remained in treatment for longer durations than those on MOUD alone (gray bars). These findings underscore the magnitude of improvement in both abstinence and retention when a digital contingency management approach is added to standard care.
- Interpretation: The study’s authors concluded that “augmenting medication for opioid use disorder with app-based contingency management may provide clinical benefits” for patients. Even in a real-world, underserved patient population, those who engaged with the smartphone app’s reward program achieved better outcomes than those who did not. This suggests that the motivation and structure provided by the app can enhance the effectiveness of MOUD, helping patients reduce their opioid use and remain in care. Notably, the benefits were observed without requiring intensive clinic-based counseling or frequent in-person visits – a testament to the power of a well-designed digital intervention. The researchers emphasized that expanding access to app-based CM could help “decrease the immense societal, economic and personal burden of opioid use” by improving recovery success rates. In summary, the study provides robust evidence that digital CM is a feasible and effective augment to medication treatment in community settings.
Clinical and Economic Implications
The positive results from this study have significant clinical and economic implications for addiction treatment systems:
1. Improved Patient Outcomes and Recovery Rates: From a clinical perspective, the addition of app-based contingency management led to measurable improvements in key outcomes that drive recovery success. Fewer days of opioid use at end of treatment indicate that patients in the app group achieved higher levels of abstinence, or at least more prolonged periods of sobriety, than those on MOUD alone. This reduction in use is clinically meaningful – every day not using opioids is a day with lower risk of overdose, infectious disease transmission (e.g. HIV/HCV), or other complications of use. Furthermore, longer retention in treatment is strongly correlated with better long-term outcomes in OUD. Patients who stay engaged in care are more likely to achieve stable recovery, as they continue to receive medication and support for a sufficient duration. In the study, the app group’s 19% increase in treatment duration could translate into higher rates of sustained abstinence beyond the study period. Clinicians understand that retention is often half the battle in addiction treatment – thus, a tool that keeps patients coming back and adhering to therapy has immense value. By enhancing both abstinence and retention, digital CM tackles two of the most critical challenges in OUD care.
2. Addressing Gaps for Underserved Populations: The cohort in the study consisted largely of uninsured or underinsured individuals, a group that faces numerous barriers to accessing quality addiction treatment. The success of the app-based intervention in this population is particularly encouraging for public health efforts. It demonstrates that technology can help bridge the treatment gap for vulnerable groups. A smartphone app is relatively low-cost and can be distributed at scale, making it possible to reach patients who might not have the resources or ability to attend intensive in-person programs. By providing recovery support and incentives through a device most people already own, digital CM can extend the benefits of evidence-based treatment to those who traditionally have been left out. This is crucial considering that only ~1 in 5 people with substance use disorders receive treatment at all. Digital platforms like WEconnect can be deployed in community clinics, opioid treatment programs, or even via public health initiatives to engage patients who are often hard to keep in care. In essence, app-based CM can act as a force-multiplier for MOUD, improving outcomes broadly and equitably.
3. Economic Benefits and Healthcare Cost Savings: The opioid epidemic imposes huge costs on healthcare systems, insurers, and society. Effective treatments that reduce drug use and promote recovery can substantially offset these costs. For instance, patients with untreated SUD frequently cycle in and out of emergency departments and hospitals, incurring high acute-care costs. By keeping patients in treatment and reducing relapse, app-based CM has the potential to lower utilization of expensive healthcare services (fewer overdose reversals, hospitalizations, etc.). Additionally, every opioid-free day and every additional month in recovery likely reduces involvement in criminal justice and increases productivity, yielding economic benefits beyond healthcare. MOUD alone has been shown to be cost-effective by reducing crime and health costs; augmenting MOUD with CM could further amplify these savings. One economic analysis of traditional CM found a high probability that the benefits of CM outweigh its costs in addiction treatment. Digital delivery can make CM even more cost-efficient: automated apps minimize staff labor and clinic infrastructure needs, meaning low marginal cost to support each additional patient. In the study, the rewards given to patients were modest (often small incentives), yet the return in terms of improved outcomes was significant. Payers – including Medicaid programs, commercial insurers, and state agencies – should take note that investing in digital CM may pay off by reducing total cost of care for OUD patients. The clinical improvements translate to economic value in the form of fewer adverse events and more stable, healthy individuals contributing to society.
4. Feasibility and Scalability of Digital CM: A major takeaway is that contingency management can be delivered successfully via a digital platform in real-world settings. This addresses longstanding feasibility concerns that limited CM adoption in the past. With the WEconnect app, patients were able to engage with CM without burdensome clinic schedules, and providers could monitor progress through the app’s dashboard. The high retention in the app group suggests that patients found the digital intervention acceptable and worthwhile. This bodes well for scaling up such programs: technology-enhanced CM offers “widescale access to an evidence-based treatment with low staff burden, no side effects, [and] high fidelity” in implementation. Once the app infrastructure is in place, enrolling more patients is straightforward, as the system automates goal tracking and reward delivery. Geographic scale is also achievable – the Texas study spanned multiple clinics, and a cloud-based app can serve rural and urban areas alike as long as cellular or WiFi service is available. For policy-makers and provider networks, this means digital CM is a scalable intervention that can be rolled out across regions or state-wide with relative ease compared to brick-and-mortar programs. It aligns well with telehealth expansion trends and can be integrated into existing telemedicine or digital care management offerings.
5. Shaping Clinical Practice Guidelines: As evidence accumulates (including this study’s results), there may be shifts in official guidelines and best practices for OUD treatment. Organizations like SAMHSA, NIH, and professional societies may begin to recommend contingency management as a standard adjunct to MOUD for appropriate patients. In fact, federal agencies are already funding and encouraging the adoption of CM, especially given its strong evidence base in treating stimulant use disorder. Digital delivery via apps like WEconnect could accelerate acceptance by offering a practical modality to implement these recommendations. Clinicians should become familiar with app-based CM tools and how to incorporate them into treatment plans. Similarly, training programs for addiction counselors and peer support specialists can include modules on using digital platforms to engage clients. The ultimate goal is that in routine practice, a patient starting MOUD would also be offered enrollment in a digital support app that provides contingency management and recovery coaching, thereby making integrated care the new norm in battling opioid addiction.
In summary, the integration of app-based contingency management with MOUD represents a promising advancement in OUD care. The clinical improvements observed – significant reductions in drug use and better retention – directly address key failure points in treatment. For healthcare systems and payers, these improvements likely translate into cost savings and better allocation of resources. And for patients, especially those facing socioeconomic barriers, digital CM lowers the threshold to participate and stay engaged in life-saving treatment. The next section will discuss how WEconnect Health’s platform exemplifies this digital approach and what differentiates it as a leading solution in the market.
WEconnect’s Differentiation in Digital Addiction Treatment
Technology is rapidly transforming how we deliver behavioral health interventions, and WEconnect Health has positioned itself at the forefront of this movement in addiction treatment. The recent study’s success is not only a validation of contingency management as a concept, but also a proof-point for WEconnect’s specific approach to designing and deploying a recovery support app. Several attributes distinguish WEconnect’s digital platform from other treatment modalities and even from other apps in the space, making it especially effective for engaging patients:
Figure: The WEconnect mobile app provides recovery support through an intuitive smartphone interface. The screenshot above shows examples of its features: personalized daily goals and inspirational quotes to motivate users, a “Rewards earned” display (e.g. a $10 incentive) that reflects contingency management bonuses for completing activities, and tracking of meeting attendance and other healthy behaviors. The app’s user-friendly design encourages patients to interact with their recovery plan daily, earning immediate positive reinforcement for progress.
Comprehensive Recovery Toolkit in One App: WEconnect’s platform combines multiple support components in a single, easy-to-use application. Evidence-based CM is embedded within a broader “recovery-oriented framework” – meaning the app is not solely about giving rewards for negative drug tests, but holistically supports the user’s recovery journey. Patients can set daily goals that are meaningful to them, spanning both substance-use targets and general wellness activities. For example, through the app a patient might pledge to attend a Narcotics Anonymous meeting, take a morning walk, or spend time with family, in addition to maintaining sobriety. Progress on all these goals can be recorded in the app, helping patients build routines that support recovery. The integrated approach (combining incentives, self-management tools, and peer support) differentiates WEconnect from many single-feature apps.
Personalized Incentives and Goal-Setting: A cornerstone of WEconnect’s system is that it allows patients to choose their own recovery goals and rewards, which enhances engagement. Traditional contingency management often focuses narrowly on clinic-defined outcomes (like clean urine screens). In contrast, the WEconnect app lets individuals decide which daily or weekly objectives matter most to them – fostering a sense of ownership in the process. When they achieve those objectives, they receive immediate positive reinforcement in the form of points or monetary rewards displayed in the app. This personalization is powerful: by tailoring goals to each user’s life (whether it’s “attend group therapy on Tuesday” or “visit with a sober friend”), the incentives align with intrinsic motivations. The study noted that app participants received “monetary incentives upon achieving their self-chosen recovery goals.” This patient-centric model likely contributed to the high retention, as users remained active to pursue goals that they themselves set, rather than feeling the program was externally imposed.
Real-Time Progress Tracking and Feedback: The WEconnect app provides real-time tracking of a patient’s activities and progress, serving as a constant feedback loop. Participants can see their streak of days without opioid use, track how many meetings or exercises they’ve completed that week, and visualize progress toward their rewards. This kind of instant feedback is known to reinforce positive behavior – the user doesn’t have to wait until the next clinic visit to receive praise or points; the app gives kudos right away for each accomplishment. Automated payment and reward delivery through the app is another key feature. When a goal is met, the app triggers the incentive (for example, adding $5 to a rewards balance), which the patient can immediately see under “Rewards earned.” This immediacy and transparency help sustain motivation. Moreover, clinicians or peer coaches can also monitor patient dashboards and celebrate successes or address lapses in near real-time, enabling more responsive care than the traditional weekly check-in.
Peer Support and Connectivity: Recovery is not a solo journey, and WEconnect recognizes the importance of peer support in sobriety. The app includes access to 1-on-1 peer support as well as daily online recovery meetings facilitated by certified peer specialists. This social support layer is a unique differentiator – users can connect with others who have lived experience of addiction and recovery. At any time, someone struggling can reach out through the app to a peer coach for encouragement or advice. There are also scheduled virtual meetings (similar to AA/NA meetings but online) that app users can join for free. By integrating these peer services, WEconnect ensures that users never feel alone; help and camaraderie are just a click away on their phone. The combination of contingency management + peer networking is powerful: incentives get patients in the door and reinforce behaviors, while peer relationships provide the empathy, understanding, and hope that keep people engaged for the long haul. This mirrors the effective components of comprehensive treatment programs, but delivered digitally.
Accessibility and Convenience: A critical advantage of WEconnect’s app-based model is its high accessibility. Because support is delivered via smartphone, patients can engage with their recovery program anywhere and at any time – at home, during a work break, or whenever cravings hit – rather than being tied to clinic hours. The app is available 24/7, which is particularly important for a chronic condition like addiction where support needs can arise outside of 9–5. This flexibility removes many barriers that commonly hinder treatment participation: there’s no need to arrange transportation or childcare to attend an appointment just to receive a reward or attend a meeting. Rural patients or those living far from treatment centers can fully participate as long as they have cell service. WEconnect’s digital platform thus “permits patients to make decisions regarding their own goals for treatment and to explore recovery through peer support services available anywhere and accessible outside of normal clinic hours.” In contrast to traditional CM that might require three clinic visits a week, the app brings the support to the patient’s fingertips. This patient-centric convenience likely contributed to the improved retention observed – treatment fit into patients’ lives, instead of forcing patients to bend their lives around treatment.
Data-Driven Insights and Customization: Another benefit of a digital solution like WEconnect is the rich data it generates, which can be used to further personalize care. The app securely records data on which incentives work best for which patients, what times of day users engage, which goals are most popular, etc. Providers and program administrators can use this data to refine treatment strategies (for example, identifying if a patient is missing goals on weekends and intervening accordingly). Over time, aggregated data can demonstrate outcomes and cost savings to payers, building the case for broader implementation. WEconnect, as a tech platform, can also iterate quickly – updates and new features can be pushed to all users to continuously improve the efficacy and user experience. This agile, data-driven approach keeps the intervention at peak performance, something static in-person programs struggle to achieve consistently.
In sum, WEconnect Health’s solution distinguishes itself by being evidence-based, patient-centered, and scalable. The app’s design intelligently combines contingency management with holistic recovery support, making it a powerful adjunct to medical therapy. The JAMA Network Open study highlighted that when given the choice, many patients opted to use the app, and those who did experienced better outcomes. This speaks to the real-world appeal and impact of WEconnect’s platform. As addiction treatment increasingly embraces digital health, WEconnect has a proven, ready-to-deploy tool that can lead the field in improving outcomes for individuals with opioid use disorder.
Conclusion
The evidence is clear: augmenting MOUD with app-based contingency management can significantly improve treatment outcomes for opioid use disorder. The integration of financial incentives, personal goal-setting, and peer support via a user-friendly app addresses critical gaps in traditional treatment – helping patients stay drug-free and engaged in care longer. For healthcare providers, payers, and policy-makers, this represents a promising path forward in the fight against the opioid epidemic.
Now is the time to translate these findings into practice and policy. WEconnect Health’s digital platform offers an immediately available means to implement contingency management at scale, backed by clinical data demonstrating its effectiveness. We urge stakeholders in the addiction treatment ecosystem to take the following actions:
- Healthcare Providers & Programs: Incorporate digital CM into standard care. Providers running opioid treatment programs or clinics should consider offering the WEconnect app (or similar digital CM tools) to patients as a routine part of MOUD treatment. Frontline clinicians can educate patients about the app and encourage its use as a way to stay motivated between appointments. Treatment programs might formally integrate app-based goal tracking and incentives into their care protocols, with staff monitoring patients’ progress through the app’s clinician dashboard. By normalizing technology-assisted recovery support, providers can enhance the quality of care and patient satisfaction. The study discussed here shows that patients are receptive to such tools – when given the choice, they used them and benefitted.
- Payers (Insurers, Medicaid, Employers): Support and incentivize use of digital recovery tools. Payers should recognize that covering digital interventions like WEconnect’s app can yield downstream savings by improving outcomes. This could include reimbursing providers for digital CM programs, subsidizing app subscription costs for members, or incorporating these tools into value-based care models for OUD. Several insurers and state Medicaid programs have begun pilots to fund contingency management given its high efficacy; these efforts should be expanded and made permanent. Employers and Employee Assistance Programs (EAPs) can also adopt such apps for workforce behavioral health initiatives. Investing in proven digital health solutions is fiscally prudent when weighed against the exorbitant costs of untreated addiction.
- Policy Makers & Regulators: Enable scaling of contingency management. Policy makers should update guidelines and regulations to facilitate wider adoption of CM, especially via digital platforms. This may involve clarifying legalities around providing incentives to patients (historically, strict interpretations of anti-inducement laws hampered CM; recent federal guidance has opened pathways for CM in stimulant use disorder treatment). Policymakers can further encourage innovation by funding grant programs and research into digital therapeutics for SUD. On a systems level, including digital CM in federal treatment guidelines (SAMHSA, NIDA best practices) and quality measures can drive adoption. State agencies might integrate apps like WEconnect into public opioid treatment infrastructures or recovery support services. The overarching goal should be to make evidence-based digital support a standard option available to all patients alongside medication and counseling.
- Communities & Advocates: Embrace technology as a recovery ally. Community organizations, recovery coaches, and family advocates should view tools like the WEconnect app as additions to the recovery toolkit, not replacements for human care but as enhancers. Stigma around addiction can sometimes extend to skepticism about “giving rewards to people with SUD”; advocacy is needed to educate the public that contingency management is a scientifically validated treatment that treats addiction like the chronic medical condition it is – using positive reinforcement, not punishment, to support behavior change. Success stories from individuals who have used digital CM to turn their lives around can be amplified to build support for these methods. By championing innovation, communities can help break down resistance to new modalities and accelerate their adoption.
In closing, WEconnect Health has demonstrated leadership in digital addiction treatment by delivering a platform that effectively operationalizes contingency management in everyday care. The 2024 JAMA Network Open study adds to the growing validation of this approach, showing that even in a challenging, real-world population, technology can help achieve better outcomes in opioid use disorder treatment. The path ahead is one of implementation and expansion. We invite healthcare leaders and stakeholders to partner with WEconnect Health in bringing this solution to scale. Together, we can create a future where fewer people are lost to opioid addiction and more individuals achieve the stable recovery they deserve – by uniting the best of medicine with the best of technology for the benefit of patients.
To learn more about integrating WEconnect’s digital contingency management platform into your treatment program or health plan, please contact WEconnect Health. By taking action today, you can help transform addiction treatment, improve lives, and reduce the human and economic toll of the opioid crisis.
Emphasize your product's unique features or benefits to differentiate it from competitors
In nec dictum adipiscing pharetra enim etiam scelerisque dolor purus ipsum egestas cursus vulputate arcu egestas ut eu sed mollis consectetur mattis pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus mauris aliquam ornare nisl purus at ipsum nulla accumsan consectetur vestibulum suspendisse aliquam condimentum scelerisque lacinia pellentesque vestibulum condimentum turpis ligula pharetra dictum sapien facilisis sapien at sagittis et cursus congue.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Incorporate statistics or specific numbers to highlight the effectiveness or popularity of your offering
Convallis pellentesque ullamcorper sapien sed tristique fermentum proin amet quam tincidunt feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Use time-sensitive language to encourage immediate action, such as "Limited Time Offer
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
- Pharetra curabitur et maecenas in mattis fames consectetur ipsum quis risus.
- Justo urna nisi auctor consequat consectetur dolor lectus blandit.
- Eget egestas volutpat lacinia vestibulum vitae mattis hendrerit.
- Ornare elit odio tellus orci bibendum dictum id sem congue enim amet diam.
Address customer pain points directly by showing how your product solves their problems
Feugiat vitae neque quisque odio ut pellentesque ac mauris eget lectus. Pretium arcu turpis lacus sapien sit at eu sapien duis magna nunc nibh nam non ut nibh ultrices ultrices elementum egestas enim nisl sed cursus pellentesque sit dignissim enim euismod sit et convallis sed pelis viverra quam at nisl sit pharetra enim nisl nec vestibulum posuere in volutpat sed blandit neque risus.
Vel etiam vel amet aenean eget in habitasse nunc duis tellus sem turpis risus aliquam ac volutpat tellus eu faucibus ullamcorper.
Tailor titles to your ideal customer segment using phrases like "Designed for Busy Professionals
Sed pretium id nibh id sit felis vitae volutpat volutpat adipiscing at sodales neque lectus mi phasellus commodo at elit suspendisse ornare faucibus lectus purus viverra in nec aliquet commodo et sed sed nisi tempor mi pellentesque arcu viverra pretium duis enim vulputate dignissim etiam ultrices vitae neque urna proin nibh diam turpis augue lacus.
%202.svg)